#250 Hybrid robotic radical cystectomy with intracorporeal conduit- Dr. Vipin Tyagi
This is one of the 2023 KS International Innovation Awards videos selected for inclusion in the Vattikuti Foundation – ORSI Humans on the Cutting Edge of Robotic Surgery Conference, October 6, 7 & 8, 2023 in Ghent, Belgium. Posting does not imply that is has been selected as a Finalist, just that the content will be discussed at the Conference.
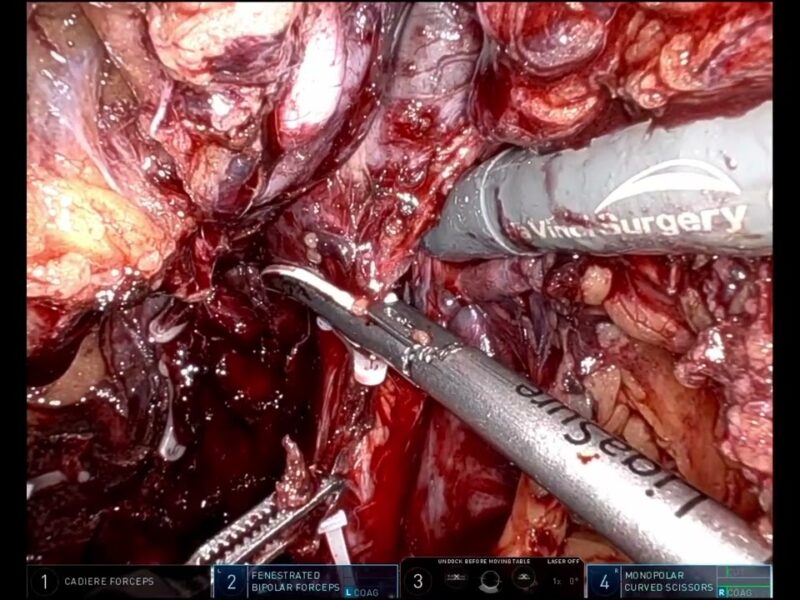
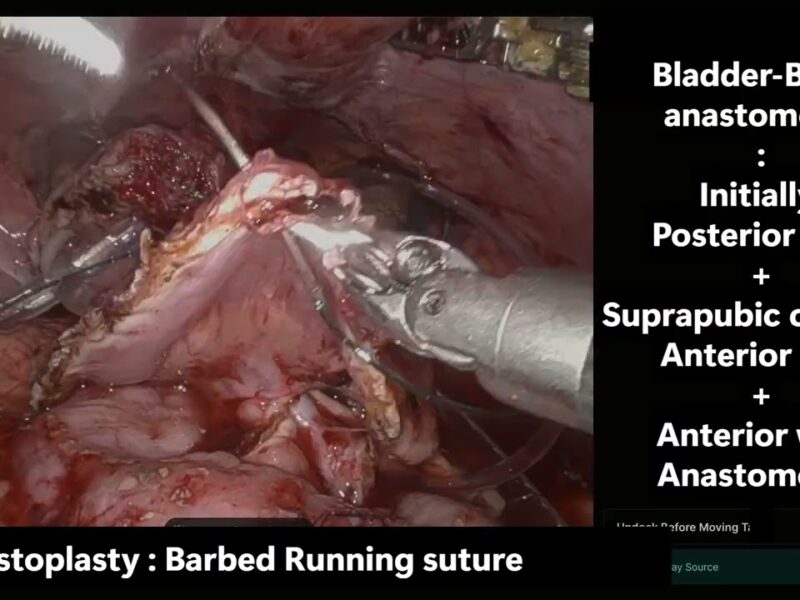
From the entry: Description: Robot-assisted radical cystectomy (RARC) may reduce morbidity after cystectomy. Descriptions of the surgical techniques of RARC with intracorporeal urinary diversion are sparse. We will be describing our hybrid technique of this complex procedure in consecutive 61 cases with oncology and functioning outcome as well as complications.
Abstract:
Introduction — Robot-assisted radical cystectomy (RARC) may reduce morbidity after cystectomy. Descriptions of the surgical techniques of RARC with intracorporeal urinary diversion are sparse. We will be describing our hybrid technique of this complex procedure in consecutive 61 cases with oncology and functioning outcome as well as complications.
Material and Methods — Single-surgeons team did RARC In consecutive 61 selected patients with high- grade and/or muscle-invasive urothelial cancer of the bladder from 2014 to 2023. Perioperative variables, pathology data, early and late complication rates, stoma function and cancer-specific survival were evaluated as outcome measures.
Results— The study population (n=61) consisted of 58 males and 3 females, aged 38-76 years. Disease profile included stages T2, T3a or T3b as confirmed by biopsy. Mean Operation time was 360 minutes. Laparoscopic bowel harvesting for the ileal conduit was completed in mean time of 45 minutes. Uretero-ileal anastomosis was done by Bricker technique. Intra- operative blood loss was estimated to be average 180 ml. There were no intra-operative or immediate post-operative surgical complications except 3 which have complication within 90 days of surgery. Patients were discharged between post-operative day 4 to 14 days. No mortality directly attributable to the surgery was reported. Most of the patients found to have pathological stage pT2 to pT3b with one patient has stage pT4.
Conclusion— Our technique of Hybrid procedure is good for surgical success with complementary use of laparoscopic and robotic advantages.
See more at: https://vattikutifoundation.com/videos/
Date
August 15, 2020