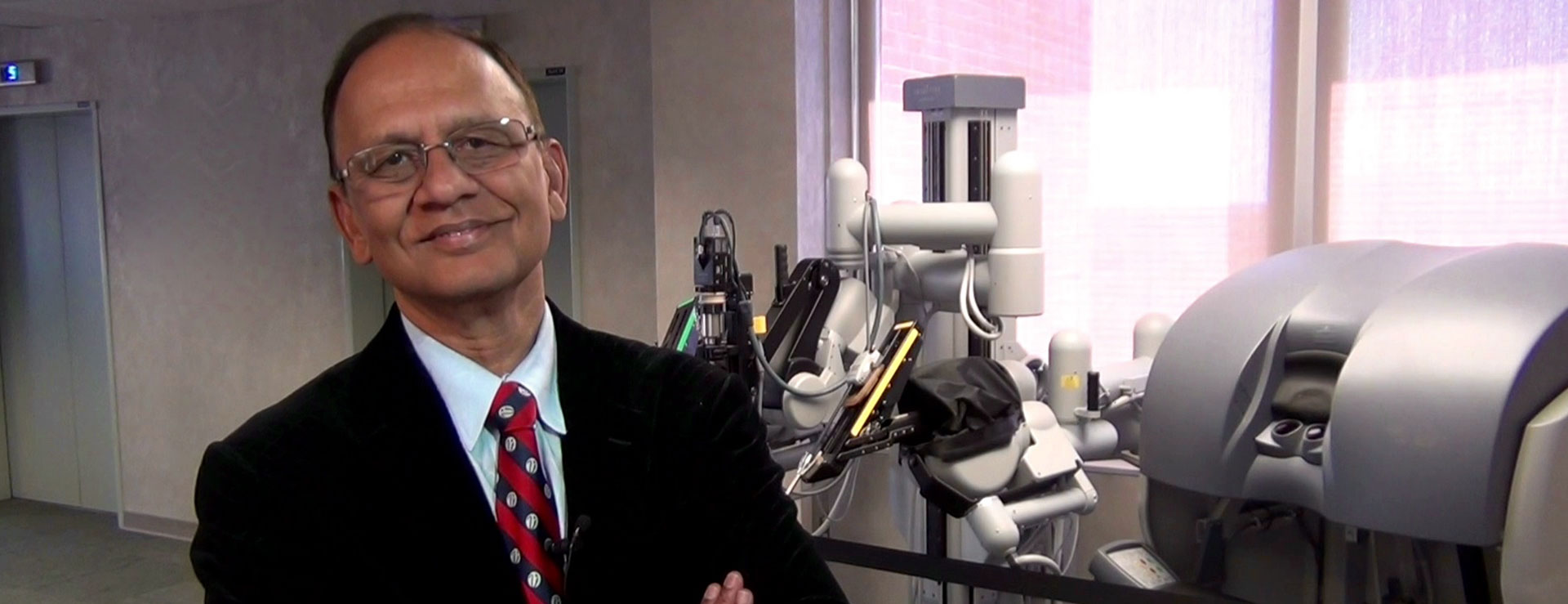
M. D. | Director
Dr Mani Menon
Vattikuti Urology Institute (VUI), Henry Ford Health System
Mani Menon, MD was the Founding Director of the Vattikuti Urology Institute and an integral partner of the Vattikuti Foundation in its programs in robotic surgery. As of July, 2021, he is a Professor of Urology at Mount Sinai Icahn School of Medicine in New York and Chief of Strategies and Innovation in the Department of Urology.
Dr. Menon has personally performed over 6000 cancer operations and is considered to be one of the foremost surgical innovators in the world. His pioneering work in robotic surgery has transformed the world of surgery.

Dr. Menon graduated from JIPMER, Pondicherry in India and completed his residency at the Brady Urological Institute at the Johns Hopkins Hospital in 1980. He served on the faculty at Washington University in St. Louis from 1980 to 1983, when he was appointed the Founding Chairman and Professor of the Division of Urological and Transplantation Surgery at the University of Massachusetts Medical School, becoming the youngest Chairman in the country at that time. In 1997, Menon became Chairman of the Department of Urology at Henry Ford Hospital and in 2000, was appointed the first Director of the Vattikuti Urology Institute.
Early Years
Dr. Menon’s early interests were in reconstructive surgery for complex renal stones, while his research interests were in renal physiology and in the biology of the prostate. At Henry Ford Hospital, he started incorporating computer-integrated surgical systems into clinical practice and established the first cancer-oriented robotics program in the world. Working with his colleagues, Ashutosh Tewari, Alok Shrivastava, Ashok Hemal and Akshay Bhandari, he developed techniques that revolutionized the field of urological oncology and laid the framework for the extension of robotics to other surgical disciplines. In 2013, Menon extended the uses of computer-integrated systems to the field of kidney transplantation. Working with Prof Rajesh Ahlawat, the Medanta/ the Vattikuti Foundation technique of Robotic Kidney Transplant has been successfully adopted at multiple institutions across the world.
Achievements
Dr. Menon is the recipient of several awards, including: The Gold Cystoscope award of the AUA; The Dr. B.C. Roy Award from President of India (which is the highest award given by the Government of India for achievements in Medical Science); The Hugh Hampton Young Award (AUA); The Keyes Medal (recognized as the greatest individual citation awarded by the American Association of Genitourinary surgeons) and The St. Paul’s Medal from the British Association of Urological Surgeons. Some of Dr. Menon’s personal effects have been displayed in the Smithsonian National Museum of American History as a permanent exhibit (2017-2036). He has been a Visiting Professor at over 50 institutions across the globe, where he has lectured, performed robotic surgery and trained hundreds of surgeons. Dr. Menon’s team has been involved in the establishment of over 35 robotic surgery programs in Europe, Asia and the Americas.
Publications
Dr. Menon has published over 1000 manuscripts, book chapters and abstracts, primarily in the field of robotic surgery, kidney transplantation, and urolithiasis. His work has appeared in the major urological journals as well as in the Journal of Clinical Investigation, the Journal of Biological Chemistry, the American Journal of Physiology, Proceedings of the National Academy of Sciences and the New England Journal of Medicine. Dr. Menon is profiled in the Best Doctors of America. He is a member of the American Association of Genito-Urinary Surgeons, the Clinical Society and the Society of Scholars at Johns Hopkins University, his alma mater. He is an honorary member of both the American Urological Association and the European Association of Urology, a recognition reserved for their most distinguished members.
Menon’s latest innovation has been the introduction of precision surgery for the treatment of prostate cancer. Through extensive modeling studies performed with Vattikuti Foundation Fellow Dr. Sohrab Arora, and the HFHS Pathology Department, Menon determined that the prostate capsule was free of cancer in 80% of men. He developed a 3-D method of sampling the capsule that identified such men with over 90% accuracy. He then developed a precise technique of prostatectomy that allowed for preservation of the capsule. This modification results in far superior functional outcomes, such as erections and urinary control. For men who are interested in maintaining their quality of life, the Precision Prostatectomy is truly a game changer.
Dr. Menon continues to accept new patients and refine his surgical procedure at his new home at Mount Sinai Medical Center, NY, NY.
Previous News Articles
15 Years Since the First Robotic Prostatectomy by Dr. Mani Menon at the VUI – November 24th, 2015

November 29th 2015 marks the fifteenth anniversary of Dr. Mani Menon performing his first Robot Assisted Radical Prostatectomy, which soon became known as the Vattikuti Institute Prostatectomy, or VIP. Recently, the Vattikuti Urology Institute (VUI) held a reunion of current and former staff and students that coincided with the Centennial Anniversary Celebration of the Henry Ford Hospital/Health System. We interviewed many colleagues of Dr. Mani Menon, VUI Chair and the person responsible for developing and performing the first robotic prostatectomy procedures at the VUI. In celebration of this surgery milestone, we will be releasing parts of these interviews, starting with Dr. James O. Peabody, the current Vice Chair of Urology at the VUI. Dr. Peabody was there at the VUI, participating right from the start.
VF: It’s amazing- the ingenuity of Dr. Menon. What it has turned into for the whole medical field.
Dr James O. Peabody: Yeah - he had the vision. It was kind of a ‘perfect storm’ sort of thing. The elements- as I see it- were Mr. and Mrs. Vattikuti, who wanted to fund an innovative prostate cancer research program, because without their generous support, this would still be a dream, to a large degree.
There is Dr. Menon, who wanted to find a better way to treat prostate cancer patients. Laparoscopic surgery was sort of just coming on the horizon as something that could be done and he had the vision to go and contract with the best laparoscopic surgeons in the world to come and work with us. As they arrived, the robot was just being approved, and it was suggested, through some discussions, that we try to get a hold of a robot to see what we could do with it, while they were there. So we really had a perfect team put together. And it was funded. And we did the first cases now, just about 15 years ago, as we talked about.
And I remember Dr. Tewari, Dr. Menon and I sitting in his office, and as I recall, it was January of 2001, and we didn’t have a robot at that point- we leased it- and he said “Should we buy one?” And as he tells the story, he was outvoted 2-to-1. Dr. Tewari and I said ‘Yes,’ and he wasn’t so sure, but I think he really wanted to go ahead and get it anyway- he just wanted some reassurance that was a good thing to do. So, we went ahead and got it.
It came in March. And we still, we needed some work to try to figure out how to do it. We were still learning the laparoscopic procedure to some degree, under the tutelage of the French surgeons. (Vallancien & Guillonneau)
It was really critical that we did it that way, because these guys were world experts in doing laparoscopic surgery, and we were pretty good open surgeons, but this was a whole new technology. So that coming together of all these different skills really is what enabled us to kind of push through and make it work. And then once we realized we could do it, then we started to try and do it better and better. And the operation we do now is really dramatically different than the operation we did 15-years ago. A lot of instrumentation is different. The robots are different, the approach- our understanding of anatomy, which has evolved over time, and some, through our own discovery, some through interactions and discussions with other people who we had a hand in training- earliest exposing to the technology initially, so it’s all come together, and that the field really took off. I think we did half- or more of robotic prostatectomies in the U. S. the first couple years, and then other places started doing it. So we kept doing more cases, but many other people kept doing other cases, so our percentages of cases diminished.
As I recall, the first year, we did 200 or so, and there may have been 3 or 4-hundred done in the U. S. And there were 70,000 prostatectomies done in those years, prostatectomies- not robotic prostatectomies. So, so now- the robotic prostatectomy is done about eighty, ninety percent of the time.
VF: I seem to remember Dr. Menon telling me that of like- the first 105 robotic prostatectomies, he did like 97 or 8.
Dr James O. Peabody: Yeah, I wouldn’t dispute that number. It was- we were certainly doing the majority of them. There were a few other places who had made an effort to do the cases beforehand. It’s a little bit like the Henry Ford automobile story. He didn’t make the first car, but he figured out how to make them efficiently. And for us, doing the operation in a reproducible way that could be taught to other people. And once we made that breakthrough and could pass it on to subsequent people, then it was just an ever-widening circle of knowledge. So now, every Resident in the country is trained how to do robotic surgery, whereas when we started, it was basically unheard of, for that to be the case.
When we started the program in 2000, I was the Residency Program Director and the Fellowship Director, which I did for several years after that and turned that over in 2007- the Residency Program, and the fellowship program just about a year ago. A little less than a year ago.
VF: So next to Dr. Menon, you two really steered a lot of careers in some incredible directions then, didn’t you?
Dr James O. Peabody: Yeah, we did, we had a great group of people, that came, not by any grand design- a little bit of design- but mostly people that came, as it turned out, were exceptionally talented, very hard working, and really had a gift for doing robotic surgery. So, The first resident who really was interested in this and kind of jumped to the thing was Dr. Ash Tewari, who is now the Chairman at Mount Sinai. He left us and went to Cornell, in New York. And was really the first guy in New York to start doing robotic surgery. So that was a lot of ground he was plowing, a lot of battles he had to fight. He left Cornell about a year and a half ago and moved to Mount Sinai, where he is further developing the program there.
The year after he was here, Khurshid Guru and Melissa Fisher were with us. Melissa’s a female Urology Fellowship and is doing some robotics with female urology.
Khurshid had spent some time learning about bladder cancer in Egypt. We had a program with the Mansoura Hospital in Egypt. He went there for about three months and came back with an interest in bladder cancer. We looked around for jobs for him when he was graduating and Roswell Park Cancer Institute had an opening. Their program had really kind of diminished over a number of years, so they had a new chairman, and the old chairman, they were looking for somebody who could come with some robotic skills. So, he had those in abundance, and came and really has had a meteoric career, just in a number of facets- a lot of innovative things that he’s been able to do. So, he’s really become a world leader in robotics.
Another guy was Ketan Badani, Mike Kumo- the two of them, were, I think, in the next year and, they did- they really did a lot of robotics with us as we were doing the cases.
That was the- sort of in the heyday of our time, when we were really so far ahead of the curve. We were doing hundreds of cases. I think 7-8 hundred cases a year, which was really an enormous number. These guys just had tremendous training, and as a result- they went out and established robotic programs.
VF: They knew how, no one else did.
Dr James O. Peabody: Right. They knew how, and every place they went, they were, defacto- the best-trained people.
So, for really about a ten-year run, we had exceptional Residents. In terms of their robotic training, being just well ahead of everybody else. Our numbers have diminished a little bit. Our Residents are still, I think, among the best-trained Residents for robotic surgery, although maybe not by quite the same margin as it was before, because we also had the opportunity to train a number of other people. We did the IRUS programs, the International Robotic Surgery symposia. I think starting in 2003, and we did uh-I think two or three years, and we took a year off, and we did another year, then we took another year off and another year. And those were really the first robotic programs in the world that were done. We had people from around the world, coming to watch our 3D projection. There are some great pictures of people in 3D glasses watching the things. I think that really supercharged a lot of interest around the world, in terms of trying to pursue robotic surgery. People could see firsthand, what we were able to do. We did a number of live surgery cases and as a result of that, we had more people coming to watch us, outside of the symposia.
I don’t think we have a complete list, but there were hundreds of people who came to visit us, uh, between 2003 and 2007 or so. We went around the world, demonstrating robotic surgery, in Asia, in Europe, in Australia. So, really, literally around the world we went. We had programs in Kuala Lampur a couple of times and several training sessions in Europe that we set up for teams who wanted to learn from us.
So, it was a very busy time, in terms of teaching. And, it was a lot of fun. It’s great to have figured something out and to be able to share it with other people who are interested and bright. There’s a lot of give-and-take, so we moved- moved the field forward. I think as a result of a lot of those encounters, made a lot of friends, over the years as well.
Vatikuti Foundation: Anything you’d like to comment on about the 15th anniversary?
Dr James O. Peabody: : It’s hard to believe it’s been 15 years. Time flies fast in a lot of different ways, but to- to think that it’s already been 15 years, which I have a 25-year career- so that means 60 percent of my career has been spent doing robotic surgery- which is hard to imagine
In the earlier days, we wrote papers, which we tried to get submitted. They were disbelieved, um, shouted down, you know, we kept at it. It was really his inner strength I think, that helped us get through this.
You really need a person like that to make a revolution happen. These things just don’t happen on their own. Sometimes in retrospect, it seems inevitable that this was going to happen, of course, but the hard work, the push, the pull to move it forward to where it’s moving down the tracks freely- was really his work, I think.
As I said before- this is really because of this ‘Perfect Storm’ of things coming together, and the engine that drove the thing is clearly him, and his vision.
-Please look for more interviews in this series as we explore the history behind the first successful robotic surgery program in the world. We sincerely thank Dr. James O. Peabody for taking time to share his thoughts with us.
© 2015 Vattikuti Foundation
Dr. Mani Menon- Musings – November 29th, 2015
DR. MANI MENON: MUSINGS
(On his role as Director of the Vattikuti Urology Institute)
October 10, 2015, a distinguished group of over 50 Urologists had gathered in Detroit to celebrate the Centennial of the Henry Ford Hospital/Health System Urology Department, which became known as the Vattikuti Urology Institute following a gift from Raj and Padma Vattikuti. Many of these surgeons had graduated after serving as Residents and Fellows, many going on to lead robotic programs in hospitals across the country. While Menon did not reflect much upon the upcoming 15th Anniversary of his first robotic prostatectomy, (11/29/2015) his leadership in the world of robotic surgery was quite present in the room. Here are some of his comments:
“I’ve been the chair here 18 years, and my legacy are the people who are in this room.
The longer you are a Chair, you realize your primary skill is to avoid getting fired. To negotiate the hot waters and the way you avoid getting fired- Jim, you’ll realize it- is uh, either by going to all the committee meetings or by learning to manipulate the numbers.
I don’t go to committee meetings, but I do know how to manipulate numbers. I did a quick calculation, and if we had 100 Residents here and, if each resident makes 400 thousand dollars a year, then- there are some outliers in Southwest Florida, but- (laughter).
We have from the Urology Department generated anywhere from one to two Billion dollars of value to the Alumni here. And so- that is a good and manipulated number. I don’t know any one of you thinks they are worth a million dollars, but- collectively, you are. And those of you who are in Residency training, you should realize, that this is worth- that you can look forward to. And- you would have touched millions of lives. Millions of people
Whether it is someone who comes in with perineal pain and anxiety, or whether it is someone who comes in with a renal cell carcinoma, or an atrial thrombus, you- or some of you, would train other people, and the legacy will go on. But without people training programs, there would be no medicine the way we see it. Patients clearly, would be worse off if this was just an apprenticeship and not a form of Residency.
There are 3 people who are involved with Residency training- one of whom is not here- Humphrey Atimo, the Residency Program Director, Jack Elder was the program Director for many, many years ago- for many, many years- for 7 years- and brought the program to accreditation with commendation. And Jim (Peabody) was the program director for 10 years before that.
My first week, I had a Russian patient who was an immigrant and, who didn’t speak much English. And he had two fairly attractive daughters. He had some renal cell carcinoma with nodes extending up into the atrium and I forget what, but he’s a big guy and a tough operation and it was not likely to succeed because he had palpable nodal disease, but he had just one request: "I want to spend the summer in Kroger, shopping for my family. If you can give me just 3 months of life- I can’t even move from the bed to the chair.
So, I said ‘We can do a palliative nephrectomy and remove the thrombus out.’
And, I booked the patient. The next thing I know is Bob- who’s Shetty’s running mate, has reported me to the Administration, saying ‘I’m doing unethical medicine, exceeding my capability.’
Now, I don’t know that it was unethical, but he might have been sharp at realizing that I had exceeded my capabilities, so- I didn’t understand why this would be- because I had been a chairman for 14 years, and- this is something that I had done, and we had written about it. I happened to have had one of the world’s greatest experiences with open surgery for atrial thrombuses at that point. So, I knew, certainly knew how to get into trouble- and most of the times- I knew how to get out of trouble.
So, I told Bob “If you feel ethically challenged by this, you shouldn’t scrub on this- I don’t want to involve your ethics.”
And I went to Dr. Cerney and Dr. Farah and I said, “Well, what should I do now? I mean, the Chief Resident, who’s under services, isn’t going to scrub on it.” Khurshid Guru, who is still roaming around there, so I didn’t know I could have called you (to Guru in the audience, who banters w/ Menon).
“You were under wraps.” (Laughter)
So Cerney said, “This is the best thing that has happened to you! Sugand Shetty will scrub on it and that patient will do fine!”
“And that’s exactly what happened. (To Shetty- in audience) Remember that? I mean, I’m abbreviating some of that, but Brad Bay, who some of you remember, went to that same Kroger and much to my surprise- he saw this gentleman for 2-years at the Kroger. So, I mean, you never know. I mean, maybe the smart thing would have been to have written him off. Certainly it was an expensive way to- allow someone.
But this is what we are about. Medicine is a profession- it’s not a business. You look after the patients. And very clearly, this is what he wanted. But there are all the nuances of ethics and I think I give a lot of credit for Bob Banzani- I was the new Chair and this was not something- according to Bob- that Urologists had done before I came. And he was strong enough that he voiced his complaints through the proper channels.
And so, I can only wonder what he would have done when I was doing robotic surgery! Which I really had no clue about.
So, Jim, I think, is an authentic ‘war hero,’ and a man of few words, um. The Robotic Program would not have existed without 3- people: Jim, Frank Holloway and Dirifat Dagger, these were the people who referred the first patients to us for- first laparoscopic surgery and then- robotic surgery.
Dr. (Mahendra) Bhandari had a distinguished career in India, where he started the department of Urology at my medical school, and then at Lucknow, A superspecialty hospital, which he then went on to lead- CEO of the medical center. Then, he went to King George’s Medical University, a university that is a couple hundred years old, and became the Vice Chancellor, completely re-vamped it… He has a dual appointment with the Vattikuti Foundation- he runs the Vattikuti Program round the world- the academics part of it, plus at VUI.
All of our residencies- I think I share what Khurshid Guru said so eloquently- the training was so important for us, and those years were critical, the people we worked with- the troubles we had anew. People pitched in and covered for us- these are parts of our- Mark, when you were saying earlier today. These are our true peers.
Jim had thought about creating a ‘Centennial Tie.’ There is a VUI tie, but some of you are ‘pre-VUI.’ I did not see a difference between VUI and pre-VUI, but that’s- perhaps that is shortsighted. VUI is not exclusionary, it just happens to be the re-naming of the department. So, we would like to create a centennial tie for this occasion. Craig Rogers and I and Jack Elder were at Johns-Hopkins Centennial, and that was one of the nice things they did. So, we’ll do it. We might have to defray… costs…
Dr. (Fred) Muhletale has agreed to defray all the expenses (laughter) and Dr. Shrivastava. Would you like to see Dr. Shrivastava’s house? Would you like to see Dr. Tewari’s son-in-law? Would you like to hear Dr. Ravi Barod? OK, Thank you.”
© 2015 Vattikuti Foundation
15-Years of Robotic Surgery at the VUI- Two Different Perspectives – December 14th, 2015

Two Vattikuti Urology Institute (VUI) surgeons- one current and one former- share their stories about working with robotic surgery pioneer Dr. Mani Menon. First, we hear from Dr. Wooju Jeong, Senior Urologist at the VUI:
WJ: I’ve been working for six years- actually September 30th (2015) is exactly six years, half working as a Fellow and half working as a Senior Urologist. I’ve been enjoying Vattikuti Urology Institute a lot, most interesting, I mean exciting part- is working with Dr. Menon. He is very innovative… His thinking as a young guy was very innovative and then very creative, and then a very adventurous surgeon. I’m learning a lot from Dr. Menon.
Not only... about surgical skills, but also learning his speed and his mind. So, all other staff here who taught me not only for robotic surgeons, but also … the surgeons as well. So, I’ve learned from Dr. Peabody and Dr. Stricker, Dr. Rogers, and then before- Dr. Azawa, and also, my ex-colleagues, all the Residents who graduated this program here. So, everybody’s training very well, treat me very well. I’m so far, I’m so happy to be a part of the Vattikuti Urology Institute.
Congratulations- 15th anniversary- I really appreciate Dr. Menon’s work here, and also very appreciate all our VUI team. Thank you.
VF: You weren’t here 15 years ago, but talk about the ingenuity, the creativity to come up with a new use for the surgical robot that basically was sitting on a shelf- not getting used.
WJ: So, one of the talents of Dr. Menon which is- he has quite a creative mind, to adopt one thing to another. Which is not adopted by other surgeons. So, he has a lot of searching- searching ability. He’s searching- not only the last five years the papers, also he’s searching to go beyond, and to find out good items– keep in mind- and he can adapt it to a new technique and a coming technique. So that is a kind of exciting.
So, I think the robot was one of his products. And also, he has done that before with his shockwave treatment for the (kidney) stone surgery. Nobody has used... the stone surgery for the shockwave machine. He applies- actually it was designed for gall bladder stones. And then, several decades ago, he -first he thinks about it then he adopts it on the stone surgery. Then he later adapted it to the surgery. That is another thing that he produced. He made it.
VF: Anything else you want to say on the anniversary? Any funny stories about Dr. Menon?
WJ: Not going there yet! (Chuckles)
Dr. Sugandh Shetty began his studies before the Henry Ford Hospital Urology Department was re-named after generous donations from Raj and Padma Vattikuti through their Vattikuti Foundation. His practice is at the William Beaumont Hospital in suburban Detroit.
VF: So, it’s been 15 years since the first robotic surgery with Dr. Menon?
SS: Well, robotic surgery is one of the neatest innovations in the treatment of prostate cancer and subsequently, all other urological cancers. That, we think of it as a ground-breaking innovation. That Dr. Menon and his team has produced. And, I am happy to be part of that in one way or the other. And, I’ve been doing robotic surgery for the last 13 years, part of that (chuckles).
VF: So, you followed along soon thereafter.
SS: Yes, I was the first Resident to graduate under Dr. Menon at Henry Ford Hospital. In fact, my graduation ceremony was at this yacht club. (The interview was conducted at the Grosse Pointe Yacht Club during the VUI Reunion dinner that was part of the Henry Ford Hospital Centennial Celebration.)
VF: You graduated just before he did-
SS: Before he did the robotic surgery, and I stayed on for two years, as attending staff. And then I left, and then, a couple years after I left, the robotic surgery started.
I think Dr. Menon is the leading robotic surgeon of the world. And he has not only done a lot of cases in the United States, he has taught this procedure to many, many established surgeons, surgeons-in-training, and so- the technique has spread widely, largely, because of his foresight as a procedure that would benefit patients. With reduced pain, reduced blood loss, and, ultimately, better recovery, and better outcomes.
VF: And, he was very generous of sharing his knowledge with other surgeons. He didn’t you know, keep it hidden. He shared it with the world, didn’t he?
SS: He did. He did share it with the world. Vattikuti Urology Institute put up a program every year called IRUS, International Robotic Urology Symposium. And that ran for about ten years, and was attended widely- members from around the world. And I attended almost every one of them. I’ve also gone and seen Dr. Menon operate, see how he deals with patients, so, it was really wonderful.
VF: Anything else you want to add?
SS: So, I want to congratulate Dr. Menon and his team for the upcoming 15th year anniversary of the first robotic surgery that he has done.
We really appreciate Drs. Shetty and Jeong sharing their thoughts with us. More interviews and videos will be featured in the upcoming weeks as we continue our look at the historic firsts in robotic surgery just fifteen years ago at the Vattikuti Urology Institute under Dr. Mani Menon.
© 2015 Vattikuti Foundation
A Look Back-15 Years of Robot Assisted Radical Prostatectomies – December 9th, 2015


Alok Shrivastava has been at the Cleveland Clinic Weston, Florida, since 2009. He is the Head of their Robotic Uro-Oncology Program. This is his interview from October 9, 2015, as the 15th Anniversary of Dr. Mani Menon’s first Robot Assisted Radical Prostatectomy was approaching (Nov. 29, 2015). Thanks to Dr. Shrivastava, we get to see an example of the serious side of Dr. Mani Menon’s method of training his Residents and Fellows at the Vattikuti Urology Institute. His recollection seems funny years later in retrospect, but back then.
VF: It’s been 15 years. Hard to believe, isn’t it?
AS: Seems like yesterday. I was fresh out of the boat, with having an accent, coming to this country, as a Fellow with Dr. Menon, with all the dreams in my eyes… I just wanted to do some experience in America and probably go back to India, and take some of the American technology back home.
While working with Dr. Menon, we ended up developing robotic procedures. For initial five years, almost everyone made fun of us: “We can do this thing with our bare hands, and you guys are using a million-dollar machine, and two thousand dollars’ worth of consumables, to do the thing which we do with our hands! You guys must be working for Intuitive Surgical!” And it was very hard to convince them that we don’t have any financial interest in Intuitive Surgical*. On the contrary (regarding) Intuitive Surgical, Dr. Menon, Vattikuti Foundation were paying a lot- towards getting their equipment.
It was such a pleasant thing to see that the same people that make fun of us in 2009, wanted to hire me at an atrocious sum of money. And, they desperately wanted someone who could do this operation. And that’s where- being “Menon-trained” really worked for us! Because, the world was right at our feet- wherever we wanted. All of us, who were Menon-trained could go and lead the program.
VF: And that’s one thing- so many of his protégé’s went on to lead programs around the country- and all around the world-
AS: And this is the outside, unique thing about the training program; it does not train Urologists; It trains the leaders! It trains people who can think, people who can innovate. People who can beat all the odds. Because, they see Dr. Menon, beating all the odds- every day they work with him. So that training really works well in the real life.
VF: Do you have any humorous stories that you remember about the early days? AS: Oh yes! Many. (Chuckles.)
VF: Some were afraid to say anything…
AS: People say that for the first case, they nearly peed in pants. I had a nearly peed-in-pants experience with Dr. Menon. It’s interesting. Dr. Menon was invited for a visiting professorship at UCSF (University of California San Francisco). And Peter Caroll**, who was one of the biggest names in Uro-oncology, invited him. And we were supposed to do a live case in front of literally whose and who of Urology.
Dr. Menon wanted me to assist, and, as he got the invitation, he called me and said, “You’re going to assist me, but make sure that we have everything which we use here, over there.” And of course, I called the place and coordinated with the Fellow there, and we made a list of things, and he promised me that all those things were there. Things, which were not there, I took them with me. Unfortunately, the Fellow told me that they had all of the sutures, and when I arrived there, they did not have the particular sutures.
Now, bunch of times when we did the surgery at Henry Ford, we replaced that particular suture with a finer suture, without any problem. So, as I arrived there and I asked the nurse, she says, “We don’t have that suture.”
So I said, “you don’t have 3.0 Monocryl, give us 4.0 Monocryl, and we’ll use it- just don’t tell Dr.Menon.” (Laughs.)
You know ‘Murphy’s Law.’ So, as the fate would have it- this time, that suture had to break two times! So even my spare suture that I kept there, broke.
Then Dr. Menon says “OK, give me another set of Monocryl 3.0.”
And the scrub tech, who did not know, because she was the lunch relief for the previous scrub tech, she says “Dr. Menon, we don’t have 3.0, you’ve been using 4.0!”
And Dr. Menon leaves the console, comes and stands next to me, where I am assisting him, and he says very calmly, he didn’t yell at me, he didn’t get upset at me, he says: “Dr. Shrivastava, what did I do to deserve this?”
And believe me- I nearly peed in my pants!
Then, we had a two-hour trip in a car to Intuitive Surgical headquarters, in a car with him. Two hours going, two hours coming back. I was beat up. And in those days, I was traveling a lot with Dr. Menon, and so I was automatically upgraded, all the time, as is Dr. Menon. And this was the first time, I hoped, for my flight from San Francisco to Detroit: “Gawd, please don’t upgrade me!”
Guess what? I was upgraded. And I got beat up for a whole six hours of flight from San Francisco to Detroit. (Chuckles.)
But you know what? Those things, which he told me, those things that I thought that: “He was tough on us.” He was tough on us for a reason. That was to prepare us for real life!
And not a day goes by, when I don’t remember, and when I don’t appreciate, and I don’t thank him that he was tough on us! I absolutely thank him every day for being that tough on us, because that’s why- everyone who’s trained at VUI is the best.
* Intuitive Surgical is the developer and manufacturer of the da Vinci Surgical System, and is based in Sunnyvale, California.
** Dr. Peter R. Carroll, MD, MPH is Professor and Chair, Department of Urology at UCSF as of this posting (12-2015).
© 2015 Vattikuti Foundation
EAU Honors VUI Director and Staff - March 22nd, 2018

At the March 2018 meeting of the European Association of Urology (EAU) Secretary General Prof. Chris Chapple honored Vattikuti Urology Institute Director Dr. Mani Menon with an Honorary Lifetime Membership. “We appreciate your contribution to Urology over many, many years and wanted to acknowledge that,” Chapple told the EAU members gathered in Copenhagen.
Dr Menon's contributions to Urology have spanned nearly 4 decades. He was the pioneer for establishing robotic surgery in Urology, started the world's first structured training program in robotic surgery at the Vattikuti Urology Institute, Henry Ford Hospital, and described the standard techniques for robotic prostatectomy (eponymously titled as Vattikuti Institute Prostatectomy), robotic kidney and adrenal surgery, and robotic cystectomy in seminal publications (techniques that have bene replicated and performed millions of times across the globe). He is an active and avid researcher, and continues to be thoroughly involved with the ongoing research projects at VUI, steer multi-institutional collaborations with other leading centers across the globe (such as Harvard Medical School in Boston and San Raffaele in Milan, Italy, to name a few), and true to his ideals, continues to perfect the technique for robotic prostatectomy (including the recently published Retzius-sparing approach). He steered and was the senior author of this study, and was intimately involved with all aspects of study design.

Also honored: Dr. Firas Abdollah, who received first prize for the best abstract by a resident-in-training for work on identifying the optimal candidates for adjuvant radiation therapy in post-prostatectomy patients with node-positive prostate cancer. Dr. Abdollah is a Robotics fellow at the VUI, and is a prolific researcher with nearly 300 publications in the field of urologic oncology. In this novel study, Firas, Deepansh and their colleagues looked at the outcomes of nearly 5500 patients with node-positive prostate cancer who had undergone radical prostatectomy between 2004-2015 across the US and were treated with adjuvant hormone therapy, and identified specific subgroups of men who would have mortality benefit with addition of adjuvant radiation therapy. this can help identify men who truly would benefit from additional radiation therapy, while at the same time sparing unnecessary treatment and morbidity of treatment in those who are unlikely to benefit from it.

VUI fellow Dr. Deepansh Dalela was awarded the EAU Hans Marberger Award 2018 for the best paper published in Minimally Invasive Surgery in Urology for his study entitled "A Pragmatic Randomized Controlled Trial Examining the Impact of the Retzius-sparing Approach on Early Urinary Continence Recovery After Robot-assisted Radical Prostatectomy". This was published in European Urology (Dalela et al. EurUrol. 2017 Nov;72(5):677-685), the highest impact factor journal in Urology (impact factor 16.3). This study provided Level 1 evidence that a novel approach of performing robotic radical prostatectomy provides faster urinary continence recovery after surgery (compared to the standard approach), which is one of the most important determinants of patient satisfaction after radical prostatectomy.

The Hans Marberger award, annually given since 2004, is named after Prof. Hans Marberger to honor his pioneering achievements and contributions to endourology and the development of urologic minimally invasive surgical procedures, and is one of the most important honor bestowed by the European Association of Urology annually. Deepansh happens to be the youngest recipient of this award, and it puts him in an elite group comprising previous recipients from Cleveland Clinic, University of Chicago and other researchers from highly respected institutions across Europe.

Our thanks to the EAU, Dr. Craig Rogers & Dr. Valeriya Aries for contributing to this report.
Photo’s courtesy Dr. Deepansh Dalela.
By: Dave Meinhard, EAU
Fifteen Years Since the First Robotic Prostatectomy-Observations by Dr. Craig Rogers – November 27th, 2015


Fifteen Years Since the First Robotic Prostatectomy by Dr. Mani Menon at the Vattikuti Urology Institute
Dr. Craig Rogers is the Director of Renal Surgery at Henry Ford Hospital and Director of Urologic Oncology at Henry Ford West Bloomfield Hospital. He was interviewed at the Vattikuti Urology Institute (VUI) dinner celebrating the Centennial of Henry Ford Hospital/Health System, home of the VUI. Additional comments are from his lecture at the VUI Urology/Henry Ford Hospital symposium the following day in Detroit (October 9 & 10, 2015).
VF: Fifteen years ago- the first robotic procedure. Were you there for that?
DR. CRAIG ROGERS: I was doing my residency at Johns Hopkins Hospital; there was a lot of talk about this. Johns Hopkins was a cancer- was a prostate cancer center at the time. And I was learning what was thought to be the most current techniques, training with the “Father” -what’s considered the father of prostatectomy, Patrick Walsh. And, I would do these big, open surgeries, and my job was to suck all the blood.
About two-thirds through my Residency, we had a Visiting Professor come from Henry Ford Hospital, Dr. Mani Menon. And he came, and was gonna show his new technique of robotic prostatectomy. And it was great skepticism amongst the faculty at Johns Hopkins. Who, you know, was coming to do this new surgery, and “was this really any good?”
“Were the results truly what he said they were?” And he gave several talks, and he withstood some very pointed questions.
VF: He was a protégé of Dr. Walsh’s, wasn’t he?
DR. CRAIG ROGERS: He was, he was. And the key was- he did his surgery. He brought his team with him, and he did the operation. And we all put on the 3D glasses. And I was sitting in the audience, watching the screen, and for the first time, I actually felt like I saw the anatomy of the operation! It was much more magnified, the clarity of the vision. And I could see structures.
And that’s when it clicked for me- that I was seeing the future of this operation! And not everyone around me thought the same way. I think some people viewed it as a threat to their skill set. But I could clearly see, that I had to find a way to learn how to do this operation. So, I approached him, and I told him that I was convinced. And he encouraged me to continue training, and embrace robotics. Hopkins had the robot, but we weren’t using it as much, but I got some experience in the latter part of my residency, but then I did a Fellowship, so I could get robotic training.
And I was still in communication with Dr. Menon, looking for a job. I wanted a job where when I finished Fellowship, I could go someplace that embraced innovation and technology. I wanted to do kidney cancer, and he had a vision of taking his successes in prostate and taking robotics to all other areas of Urology. So, I trained with the intent that I would get kidney training and robotic training and I would come back here, and that’s where I’ve been ever since.
VF: That’s one thing that was so neat- is that he was able to envision the prostate procedure, but he took it and shared it with so many other specialties. It didn’t matter- the robot would work.
DR CRAIG ROGERS: He viewed it not as a better prostate surgery, but just better surgery in general. And, once I started doing partial nephrectomy surgeries, and I tried- I’d done these open, I’d done them laparoscopically, and I could see the tremendous challenges, trying to cut a tumor out with these stiff laparoscopic instruments and trying to sew. And I realized, once we did these robotically- this was a complete game-changer! It made the surgeries so much easier, allowing patients to get a minimally invasive approach- that might have had to get a big, open surgery, or have their whole kidney removed. So, it just clicked at that point, that this was a better way to do ALL surgeries, really. Not just prostates.
(End interview, VUI lecture excerpts follow.)
DR. CRAIG ROGERS: These meetings wouldn’t even exist if it weren’t for Dr. Menon and his contributions. So, yeah, I agree, you can’t say that enough…
It’s been nice, seeing some of the alumni, and seeing all the exciting things you are doing… I feel privileged to be adopted into the Henry Ford family, really. There’s a rich tradition here, so exciting, fun hearing about all your stories, and where I came into play here- I grew up in Iowa, did my medical training at Stanford and then, while I was at Johns-Hopkins, that’s where I first had my run-in with the VUI- Dr. Menon came as a visiting professor, took his show on the road- “The circus,” as Dr. Peabody said- did a live surgery, and I was convinced, from that point on. You know, Dr. Guru talked about seizing opportunity, and at that point- I saw an opportunity. I saw that this was clearly- the way that surgery was going to go, doing robotics.
And I asked him how I could get on board with that, and he was encouraging- doing additional training. I did a training Fellowship at the National Cancer Institute- they had a robot. They were also a big referral center for kidney, and this was a good opportunity to extend the robot to the kidney and then take a position here. In fact, during my Fellowship, I was joining the VUI on trips. We went to Sunnyvale, (home of Intuitive Surgical, maker of the da Vinci robot) trying to optimize the kidney surgery. And I’m going to show some more personal photos of those trips and how this developed.
And so, once I got to Henry Ford, it involved lots of trips to Sunnyvale, several trips to Malaysia, several trips to India. And many of you have been on these trips, and may bring back memories of this, of how we developed these techniques. So, there’s Akshay (Bhandari) working on pigs. This was I think working with Dr. Elder. He was trying to work on the pediatric urology side of things.
Initially, it was learning how to place our ports, how to dock, how to use instruments appropriately, and just going through the motions. Then Danny Eun- you see him there in the background. There are so many pictures I wish I had.
So, he had been given the charge by Dr. Menon to figure out how to cool the kidney. And so, he saw it in his mind- all these ways to get ice in. And we tried to push ice through these different syringes- it just wouldn’t work.
(Interrupted by audience: “The 7-11 in Palm Bridge?”)
Yes! We bought slushies, we analyzed the “Slurpee,” how do you slurp slush through a straw? Why can’t we put that in the body? And he figured it was some combination of the sugar and the salt. So he bought all these blenders, and at the lab at Intuitive, he was like this mad scientist, pouring all these different concoctions and- the blender and mixing it up. It was amazing- it was really fun time.
And Dr. Bhandari was our leader of the whole thing- sort of the coach- taking us through this. These were brainstorming sessions with Dr. Desai, Dr. Bhandari, India.
There was also the innovation, led by Dr. Menon, of the (robotic kidney) transplant. This is with Dr. Modi, doing robotic kidney transplants in India, and Dr. Ghani, Ahlert, Wooju- the dream team here that made the transplant happen. Assisting and working on these surgeries. So, with all this experience- this helped us in developing our team and our program here at the Vattikuti Urology Institute.
So many firsts- we were invited to do the first live webcast in 2007. This webcast, we had over 60,00 people log in to that surgery. If I had known that many people were watching, I probably would’ve – my heart rate would have been off the charts on my Apple Watch as well. The first live telecast of a partial- robotic partial nephrectomy live at the AUA two years in a row. We did the first Twittered coverage of a surgery that caught national attention. And host of the first AUA hands-on course for small renal mass in 2014.
And many developments- this is just a few that have come from here. Whether it’s how to sew up a kidney- Actually, it’s integral development of things we use routinely now- the bulldog clamp, intraoperative ultrasound- many of those were developed right here, at the VUI. Whether it’s cooling the kidney, or… endovascular removal. This was the live webcast from 2007. This was Dr. Menon giving his introduction. Dr. Peabody was the moderator for this, fielding questions throughout the day. This really ‘kick started’ things, lots of national, even international attention and more people sort of wanting to catch up with us. So many of the cases that have been done here at the VUI- on the left, more the pelvic surgeries, on the right, the more kidney-related surgeries- which are now routine- we do robotically… These new tools that we’ve been a part of developing here at Henry Ford have helped us- and many others- to do this surgery.
We will be adding more interviews as we celebrate 15-years of robotic surgery at the Vattikuti Urology Institute. We really appreciate Dr. Craig Rogers sharing his story with us.
© 2015 Vattikuti Foundation
By: Dave Meinhard
Reflections on Dr. Mani Menon and 15-years of Robotic Surgery: Dr. Jack Elder – December 4th, 2015

(Fifth in a series)
Dr. Jack Elder was the Chief of Urology, Chief of Pediatric Urology and the Program Director of the Vattikuti Urology Institute (VUI) from 2007 to April 2015. He left to become Chief of Pediatric Urology for the Massachusetts General Hospital in Boston. His association with Dr. Mani Menon actually goes back to their time while training at Johns-Hopkins. He sat down with Dave Meinhard, VF video producer to reflect on the 15th Anniversary of Dr. Menon’s first Robot Assisted Radical Prostatectomy:
JE: He was two years ahead of me (at Johns-Hopkins) and he was always one of the most brilliant people, and, the most adventurous people that I knew. And we always had a goal of working together, so when the opportunity presented itself to move from Cleveland to Detroit to join VUI in 2007, I- you know, accepted that opportunity.
And one of the great opportunities was to develop a robotic surgery program for children. And it was very successful. At the time, there were only a handful of institutions in the United States performing pediatric urological robotic surgery. So, we developed a very busy program and were able to make some significant contributions.
VF: How did he guide you?
JE: It was challenging. Dr. Menon was not a laparoscopic surgeon. I was doing laparoscopy, in terms of extirpative surgery but I couldn’t do reconstructive surgery, where actually suturing- like a pyeloplasty and reconstructing the urinary tract. So, the da Vinci robot provided a platform to perform laparoscopic reconstructive procedures.
When I moved to Detroit, at Henry Ford- they didn’t know what I was doing, but they had the infrastructure to support me to develop it. And I knew what I wanted to do, but I needed support in learning the da Vinci. So we spent some time in California, at the da Vinci- at Intuitiveheadquarters, and developed procedures. Dr. Akshay Bhandari and I worked together to do that. We went as a team. Dr. Rogers went, Dr. Mahendra Bhandari also went and a few of the chief residents went.
The next month, we had a team that went to Malaysia, to Kuala Lumpur and we worked there for about two weeks. I had my own room where all I did was Pediatric Urologic robotic procedures. These were cases that had been identified from throughout the country over a period of several months. So they weren’t simple procedures, they were very complex procedures.
(VUI Renal Surgeon) Craig Rogers had his own room also, and then there was a third room where they were doing a variety of different operative procedures. So we had three da Vinci robots in adjacent operating rooms. And at the end, we held an international robotic surgical symposium with live surgery and talks and everything. So that really got me very comfortable with doing just about anything robotically.
My position has been that you can do almost anything related to the pediatric kidney, urinary or bladder, or adjacent organs robotically. You just have to choose who is the appropriate candidate for it. But with the support of the Henry Ford System, and particularly the VUI, with the Fellows, the Residents and the attending staff, it was a great collaborative effort. We developed a lot of good videos on complicated cases and won some awards for those.
VF: It’s been 15 years since Dr. Menon’s first procedure. What does that mean to you?
JE: I think he was the pioneer in using robotic surgery. And trying to identify- to really have a vision for what it might be able to accomplish and to try and identify where, why it might be advantageous, at least for urological procedures.
VF: It’s spread around the globe, hasn’t it?
JE: It has expanded exponentially in the United States, and it’s, right now in other parts of the planet- it’s expanding too… So, it really gives people- He really took surgery to the next level and I know that patients who have been treated at VUI- and elsewhere have been very appreciative of the minimally invasive nature and having surgeons dedicated to utilizing that technology.
VF: Anything else?
JE: I think it’s been- you know; I’m honored to have been at VUI and really, it was very exciting. It’s always exciting at VUI, and it was particularly exciting at the time I was there with Dr. Menon and seeing the development of novice surgeons developing into expert surgeons- and going into other institutions and leading very strong robotic programs- and being world leaders in that arena.
We really appreciate Dr. Jack Elder sharing his recollections with us as we continue to look back at 15-years of robotic surgery at the VUI, thanks to Dr. Mani Menon. © 2015 Vattikuti Foundation By: Dave Meinhard
Reflections on the 15-Years of Robotic Surgery of Dr. Mani Menon-Dr. Sanjeev Kaul – December 16th, 2015

Dr. Sanjeev Kaul is with William Beaumont Hospital, Royal Oak, Michigan. He is an Associate Professor of Urology and Director of Robotic Innovation and Training in conjunction with the Oakland University William Beaumont School of Medicine. He is also a mentor for medical schooling for the Capstone projects as part of the medical training.
VF: You’re one of the first people to work with Dr. Menon 15 years ago?
SK: One of the first few, yes.
VF: What was that like?
SK: It was very different. It was amazing, because at that time, it was groundbreaking, and we saw robotic surgery evolve, and we saw how it- tremendous improvements that were made- to the technique of robotic prostatectomy and robotic cystectomy. And we saw how the rest of the world, moved from being non-believers to believers.
VF: It was really world- changing, wasn’t it?
SK: It was world-changing, but at that time, people didn’t believe it. But now, you can see in both the magnitude and acceptance of robotics, and where it’s gone from Urology. It was just Urology back then, and now each and every field of surgery has embraced robotics and is using robotics for procedures.
VF: Were you in the OR for the first patient?
SK: No, I was not. I came here in two thousand and two. So, they’d probably done around a hundred patients here. But, even from around 2002, to 2005, or 2006, you could see the change. And the technique, the new things we did, also how the rest of the world started accepting it more and more. And you could see more and more centers that began doing it.
VF: Do you have any humorous stories about something with Dr. Menon? I know he has a good sense of humor.
SK: He does have a good sense of humor. I’m trying to think- there were a lot of funny things that happened- Everything. Dr. Menon was always… You know, back then, things were really serious. And Dr. Menon was- He’s very different now. He was, he was, so to say… very particular. Very, very particular.
VF: He worked his students hard- but they gained so much from that-
SK: Well, he worked hard himself. And, he demanded nothing less than perfection. And so- in all that- we really had a lot of camaraderie among the people who were there. We had a lot of fun, so- you were- you know, doing amazing things, and you were working hard, and you were aiming for perfection, but you were also having a great time at the same time, and that’s what made it really great.
VF: I remember somebody telling me once, one time he thought one of his Fellows was getting too burned out, and he gave them his charge card and said “Go out and do something with it!” Did that ever happen to you?
SK: No- I don’t doubt that that’s true, ‘cause, there was a lot of fun… I remember a time when you mentioned charge cards- I remember a time when there was a visiting Professor… and he gave the Residents his credit card and he asked us to take the visiting Professor out for dinner and drinks. And, I think we went a little- a little overboard with that. I don’t think he was very happy when he saw the bill (chuckles). But it was fun- you enjoy that. We were working hard, and in the end- he was O. K.
VF: Coming up on the 15th anniversary (of Dr. Menon's first robotic prostatectomy). What would you want to say to Dr. Menon?
SK: I think he’s built quite a legacy. And, I think if you look around the country, you see that the VUI and the Henry Ford torch is being carried around by all his students who he has taught. And they are- they are doing an amazing job. And you know, the name of Henry Ford and the name of Vattikuti is really flying high. ‘Cause all those people who have trained there, there’s a pedigree I think that comes out of here and the rest of the world sees it in all of the people who are out there. So, he should be extremely proud of that.
And- the other thing about him that, that really stuck with me is that which you don’t see that often. I mean, people do good things and they’re good surgeons, and they may do research. But with him, it’s like every day he gets up and you know, he’s thinking to himself, “I’m not satisfied with this. How am I going to make this better?” Which is amazing.
We thank Dr. Sanjeev Kaul for reminiscing with us. This is the final interview in the series, but there will be videos and more articles added to the VFRSI website as we remember and salute the first fifteen years of robotic surgery of Dr. Mani Menon at the Vattikuti Urology Institute.
© 2015 Vattikuti Foundation
By: Dave Meinhard
Reflections on the 15th Anniversary of the Robot Assisted Radical Prostatectomy -December 7th, 2015


The Vattikuti Foundation continues to recognize the Fifteenth Anniversary of Dr. Mani Menon’s first Robot Assisted Radical Prostatectomy. Recently, VF video producer Dave Meinhard interviewed Dr. Khurshid A. Guru, Director of Robotic Surgery at Roswell Park Cancer Institute, Buffalo, New York. He was in Detroit for the Centennial Celebration for the home of the VUI, Henry Ford Hospital. Professor Guru is a former Vattikuti Urology Institute Resident:
KG: One of the most important things I could tell you is that when the robotic prostate revolution started at Henry Ford, we were junior Residents. And, one of the issues was that- everybody wanted to do prostatectomies- and one of my goals was to learn how to do cystectomies. Dr. Menon had the vision to send me to Mansoura, which is one of the world’s most famous bladder cancer centers in Egypt, with some of the finest surgeons. After that, he brought me back and gave me strong training at Henry Ford. And the amazing part is that- I was able to kind of put these two skills together, to start a bladder program at Roswell Park Cancer Institute. And after that- everything else is history.
VF: Talk about the history. Dr. Menon’s incredible idea to use the robot for something that had never been done before.
KG: So, one of the most amazing and innovating- and kind of the most courageous thing- was that Dr. Menon went to Egypt with the robot. We had- nobody ever dared to take technology to a new place, to some of the finest bladder surgeons and kind of tried the procedure with them. And get their insight into building a new operation and pioneering work, while you have some of the most stringent surgeons looking over your shoulder and critiquing you. And that insight- almost more than a decade back, of taking the robot, and making the most critical surgeons for this procedure look over your shoulder, while you are developing your technique, I think was kind of a feat in itself.
VF: It was a true team effort then, wasn’t it?
KG: It was definitely some of the best open surgeons, with new technology, and with a visionary, together. And they build this whole idea of using the robot for bladder cancer.
VF: What would you like to say to Dr. Menon, on the anniversary of his fifteen years of robotic prostatectomies?
KG: I think one of the things I want to say to Dr. Menon is that what you see around- is basically the proof of the pudding. Fifteen years ago- fifteen years back, what he did was innovating, new, risky, kind of scary, but I think the proof is in what history did- fifteen years later. He set the bar of prostatectomy high, but he also raised the bar on the lower end.
If you look around the world, a lot of people are doing this operation very well. And the reason is because we were able to see a technique come out of Henry Ford Hospital that raised the bar to a level, where the whole lower end went up. So, the quality of this operation and the results of the operation are remarkably better and consistent with a lot of surgeons, versus fifteen years ago, when you had a few Master Surgeons in a few areas. Now this has gone- like they say- viral. With very good results.
Our sincere appreciation to Dr. Guru for giving us his thoughts on this important milestone.
© 2015 Vattikuti Foundation
By: Dave Meinhard
Reflections : 15-Years After the First Robotic Prostatectomy-Dr. Akshay Bhandari – December 2nd, 2015

November 29, 2015, was the 15th Anniversary of Dr. Mani Menon's first robotic prostatectomy surgical procedure at the Vattikuti Urology Institute (VUI). The results of this and many of his following robotic procedures have changed the way surgery is done throughout the world. Recently, during the Centennial Celebration honoring Henry Ford Hospital's 100 years of service to Detroit (October 9 & 10, 2015) we interviewed former students, plus current and former colleagues of Dr. Menon about what it was like to participate as history was being made at the VUI. This interview is with Dr. Akshay Bhandari, who spent ten years there as a Resident, Fellow, researcher and Staff Surgeon, before being called to the Mount Sinai Medical Center, Columbia University, in Miami Beach, Florida.
He is the Director of Robotic Surgery, Assistant Professor and Co-Chief of the Columbia University Division of Urology there. He was interviewed by Dave Meinhard, Foundation video producer. This is from the transcript, recorded October 9, 2015 at the Grosse Pointe Yacht Club, during a VUI Henry Ford Centennial reception and dinner:
AB: It just goes to say how far we’ve come. Amazing. It feels like yesterday when everyone looked at this procedure with a lot of skepticism. People were not sure if it made any sense or not. It’s just- it’s amazing how it’s revolutionized how surgery in general is practiced. It’s revolutionized how robotic- or how radical prostatectomy has evolved. It’s amazing what the Department under Dr. Menon, has established or has achieved in the last 15 years.
VF: There was a lot of skepticism at first, wasn’t there?
AB: There was- absolutely. I remember going to the annual meetings and not much discussion or presentation. I remember trying to get papers published and not getting accepted- very quick rejections. And it’s just changed over the last 5-6 years, I would think.
VF: Were you there for the first procedure?
AB: No, I wasn’t there. As a clinical person, I was in research. And I remember hearing about these things and being very intrigued by what it actually meant, because I hadn’t seen the robot myself. I remember longing to and wanting to be a part of it. Few years- It took me a few years after that but I still feel I was a part of a very good time and it was still- you know, establishing itself.
VF: Talk about Dr. Menon’s ingenuity- not just for prostatectomy but he went on to so many different specialties and shared?
AB: You look at Dr. Menon’s career and you know, this doesn’t surprise you. I think- a textbook example of ‘thinking-out-of-the-box’ means. He’s always looked at a problem differently, and came up with a solution. He’s put his head down and- he hasn’t bothered about what "A" has to say about it- or “B” thinks about it, if he thinks it’s right and he knows he can do it. I think the one thing that- that I always will try and remember, and try to imbibe in me is his attention to details. The amount of planning that goes into anything. I think that’s what’s important.
I remember him telling me on a lot of occasions, you know: “It’s not like rolling out of bed and coming to the OR. If you have a case that you want to do that’s not routine, you want to think about it, in advance, plan your steps, and that’s the way to succeed.” And I still try and do it, but I think no one does it better than he does.
VF: You now head your own program. What have you taken to your new program at Miami now?
AB: As I’ve said, I’ve obviously taken all the skills I’ve been given and hopefully, tried to improve upon my own skills. What we graduate with at Ford (Henry Ford Hospital/Health System, home of the VUI) is an amazing breadth of Urology. Not just robotics, but obviously in robotics- there’s so much experience we get out of it, so much confidence. And I felt it was all about the patient, all about good training, all about good Medicine. And in this day and age, I think if we can keep that- and that’s what I try to teach my residents. We have a residency program and I- I hope that I am able to train them at the same level I was trained. And that’s pretty much my goal. Because, I feel, wherever I am, I wouldn’t have been without the program, without Dr. Menon, without the other faculty who really have done an amazing job of- over the years.
VF: Anything you’d like to say to Dr. Menon to congratulate him?
AB: Sometimes words fail you. All I can say is congratulations, thank you. Thanks for doing this. Thanks for having us all together, it means a lot, and the fact that a lot of us came, makes it obvious it means a lot for us. We appreciate all you’ve done for us, for the patient. And we look forward to several more years of such contributions.
© 2015 Vattikuti Foundation
By: Dave Meinhard
Profile: Dr. Mani Menon and the MPP – October 9th, 2018


“I mean- this is a huge difference!” Robotic surgery pioneer Dr. Mani Menon, Founding Director of the Vattikuti Urology Institute exclaims as he converses with Vattikuti Foundation CEO Dr. Mahendra Bhandari about the latest project he has undertaken: The Menon Precision Prostatectomy, or MPP. Drs. Menon and Bhandari were meeting to discuss future plans to develop the procedure, based on findings from the first patient results. Holding up an orange, which the innovative robotic surgeon uses as a model of a prostate gland, he explains the basis for the MPP:
“This is an orange. Think about it as if this was the prostate gland. An orange has fruit and a peel. Similarly, the prostate has flesh (the glands) and a peel (the capsule). Cancers of the prostate start in the flesh of the prostate, in the orange, if you will, and then will gradually extend out through the ‘peel,’ before they spread outside the prostate.”
Dr. Menon points to the exterior of the fruit: “The nerves that maintain erection, are scattered through the peel of the orange- or the capsule of the prostate. In any given patient, can we find an area of the peel that does not have cancer? And, if we were able to preserve it, would we be able to preserve more nerves, and would that result in better function? And the answer to this is: Yes, yes, and yes!”
Being in the room, one can feel the passion the acclaimed surgeon (there are dozens of awards scattered around his office) has for this ongoing research. Menon has never been one to rest on previous accomplishments- he is driven to make life better for prostate cancer patients, and feels that the best treatment for prostate cancer is to remove it. He tells the Vattikuti Foundation about the data results from his first MPP patients:
“I think it’s encouraging. We’ll need to measure this more carefully; we’d like to start a clinical trial, to see exactly what patients are candidates for this, and collect the data very robustly.”
The word ‘Precision’ in the procedure title refers to the exacting way that some of the ‘peel,’ or capsule of the prostate is left behind by the surgeon- along with a bundle of nerves critical to preserving erections far better than previous prostate procedures could: First, a 3-D biopsy is done, providing the team with the locations of suspected cancer tissue within the prostate gland. Menon explains further the advantage this new diagnostic tool has helped to provide:
“There is a 3-D biopsy machine that was just approved by the FDA about a year ago. We got that machine about 6-months ago, and we have a clinical trial for doing the 3-D biopsy, and seeing if it can allow us to map the cancer better.”
He once again demonstrates with his orange: “We’ve found that we can map the cancer better. In very selected patients, all you’re doing is preserving the peel, or the capsule of the prostate. We are not leaving all of the peel behind. Let’s say that the cancer is on the right side: On the right side we would remove the entire prostate, and on the left side, we would remove the entire prostate, but leave the peel.”
So far, leaving a small part of the prostate behind is yielding big results: “We are leaving behind just 4-to-5 millimeters of thickness, but preserving that- resulted in potency rates of 85-to-95% at one year!” By comparison, removing the entire prostate results in potency rates of 25-to-40% at one year. It is important to note that the 4-5 mm capsule is left behind only if no cancer is found on pre-operative 3-D biopsies. If cancer is found throughout the capsule, the patient receives the highly regarded Vattikuti Institute Prostatectomy.
Dr. Menon cautions us that there is one caveat: “The flip side of this is: ‘OK, you’ve increased potency, but in what percentage of patients are you missing cancer in the peel? How accurate is your biopsy of the peel?’ We don’t know the answer to that. Complete prostate mapping in men who have had total prostatectomy suggest that it will be around 5-to-10%, but it may be as low as 1%, if our 3-D biopsy is precise. This is why patients will have to be followed carefully for several years.”
Good research takes time.
The Vattikuti Foundation will let readers know about further developments with the Menon Precision Prostatectomy as news warrants. For more information, please visit Dr. Menon’s website: http://manimenon.com
Images / video stills: Dave Meinhard VF
Dr. Mani Menon Honored on 20th Anniversary of the First VIP RARP – December 7th, 2020



