INTRODUCTION
Prostate Cancer and Importance of Diagnosis
Prostate cancer is the most commonly found malignant cancer in males above the age of 65 years old. It originates in the peripheral zone of the prostate. It forms when there is an abnormal and uncontrolled growth of the cells, which exceeds the rate of cell death. Diagnosis at an early stage plays a vital role in disease prognosis. There is a standard of care to identify and confirm the diagnosis of the prostate cancer, these need to be performed in a sequence.
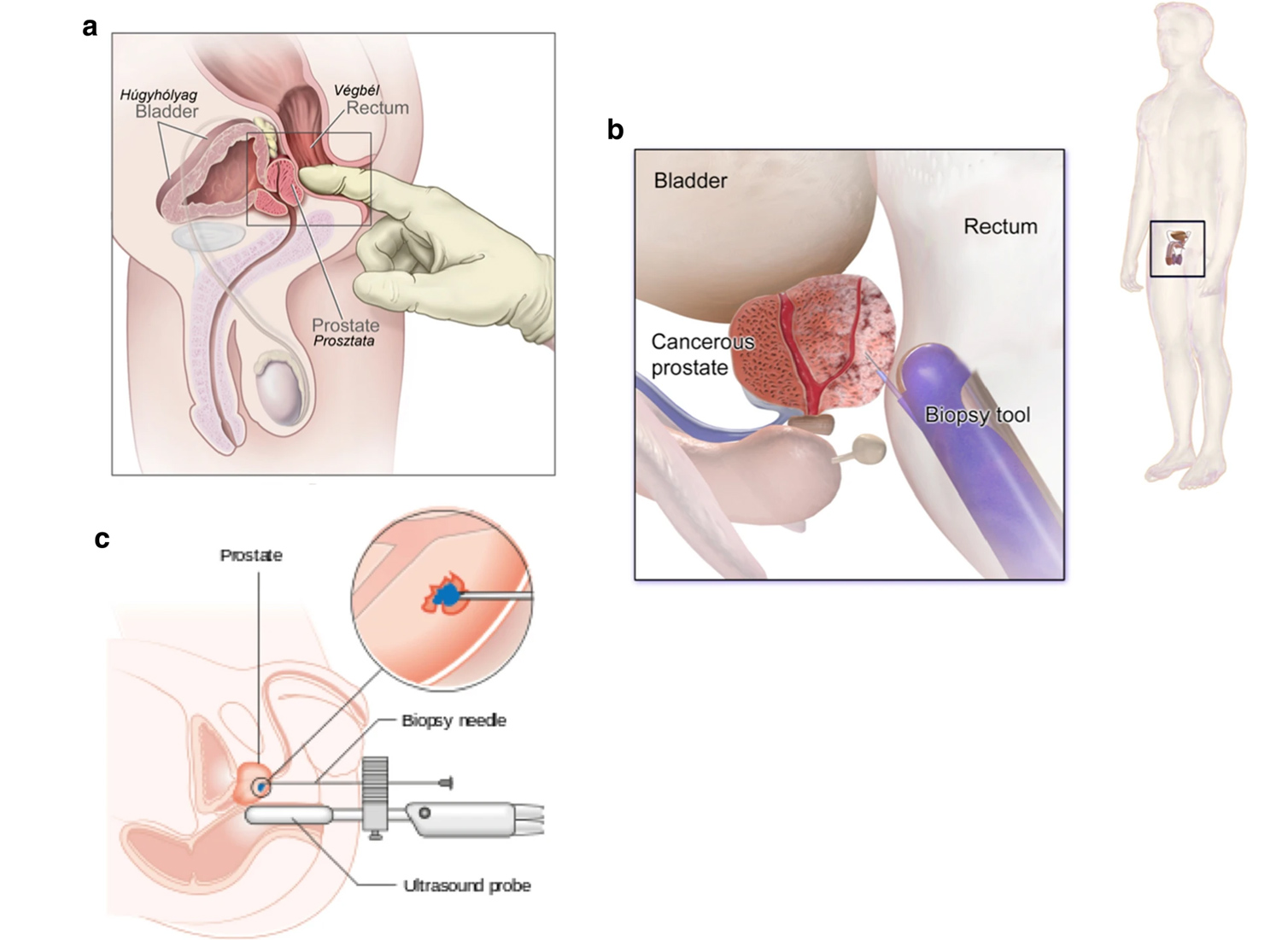
Digital Rectal Examination
Majority of early prostate cancers are not be palpable on Digital Rectal Examination (DRE). However, during DREs, tumours in their advanced stages feel like a nodular mass. The lump's surface will feel hard, nodular and irregular instead smooth surface felt in Benign Prostate Hyperplasia. Median sulcus will not be felt in Prostate cancer while it's present in Benign Prostate Hyperplasia. In the case of prostate cancer, the consistency on DRE will be heterogeneous, which means that it will not be the same throughout the gland’s surface. It might feel soft or doughy at some places while hard and lumpy on the rest. Rectal mucosa will not be able to move as it should in normal cases and will be tethered to the cancerous gland. The tissue on the side of the gland can sometimes be infiltrated, resulting in the 'winging' sign in medical terminology. This is a very significant finding on DRE in a prostate cancer patient. In your routine annual health check DRE should be an integral part to rule out prostate cancer.
More details
PSA and Biopsy
One must be wondering how we can detect and diagnose prostate cancer at an early stage when it cannot be felt on DRE. This stage is called the first stage, the T1 stage. It is further divided into three different stages. T1a and T1b are the stages at which the tumour is mostly found as an incidental finding. Incidental finding means that the prostate gland or a part of it was removed due to some other disease or pathology. Then this resected tissue is inspected under a microscope. If cancerous cells are found in this tissue under the microscope, then it is called an incidental finding. Now next stage is T1c, and it is still an early stage, so the tumour will not be palpable on DRE, but it is not going to be an incidental finding anymore. Here comes the role of Prostate-Specific Antigen (PSA) and screening.
PSA is a protein that is produced by both normal and abnormal prostate cells. Its function is to facilitate the liquefaction of semen. Though PSA is a marker for prostatic cancer but it is prostate specific, and its level increases with age normally but can also be raised in prostatic BPH cases. It is a reliable marker for the progression of advanced disease and extremely valuable in the follow up of patients after treatement or the early cancer patients who are on active survelliance However, it is neither specific nor sensitive in differentiating between early prostate cancer and BPH. In general, one should advise men aged 50-69 years to go through prostate biopsy if PSA levels are above 3ng/ml and are incremental in subsequent tests. If the tumour is identified following the investigation of a raised PSA, then it is at its T1c stage. PSA levels of greater than 2.88ng/ml and 10ng/ml are suggestive and diagnostic of prostatic cancer, respectively.