#350 PSMA-radioguided RARP with an intraoperative PET-CT specimen imager- Dr. Federico Lavagno
This is one of the 2023 KS International Innovation Awards videos selected for inclusion in the Vattikuti Foundation – ORSI Humans at the Cutting Edge of Robotic Surgery Conference, October 6, 7 & 8, 2023 in Ghent, Belgium. Posting does not imply that is has been selected as a Finalist, just that the content will be discussed at the Conference.
From the entry: TITLE: PSMA-radioguided RARP with an intraoperative PET-CT specimen imager
AUTHORS: Marco Oderda* [1], Serena Grimaldi* [2], Guido Rovera [2], Luisa Delsedime [3], Daniele D’Agate [1], Federico Lavagno [1], Alessandro Marquis [1], Giancarlo Marra [1], Luca Molinaro [3], Desireé Deandreis# [2], Paolo Gontero# [1] *Marco Oderda and Serena Grimaldi are to be considered co-first authors #Paolo Gontero and Desireé Deandreis are to be considered co-last authors
AFFILIATIONS:
[1] Department of Surgical Sciences, Urology Unit, AOU Città della Salute e della Scienza di Torino, Molinette Hospital, University of Turin, Italy
[2] Nuclear Medicine, Department of Medical Sciences, AOU Città della Salute e della Scienza di Torino, University of Turin, Italy
[3] Department of Pathology, AOU Città della Salute e della Scienza di Torino, Molinette Hospital, University of Turin, Italy
CORRESPONDING AUTHOR: Marco Oderda, MD, FEBU, Department of Surgical Sciences – Urology, University of Turin, Turin, Italy.
Phone number: +393479383465. E-mail address: marco.oderda@unito.it.
KEYWORDS: prostate cancer, robot-assisted radical prostatectomy, radioguided surgery, PET/CT, specimen imager, Ga68-PSMA-11
Word count:
1 VIDEO ARTICLE
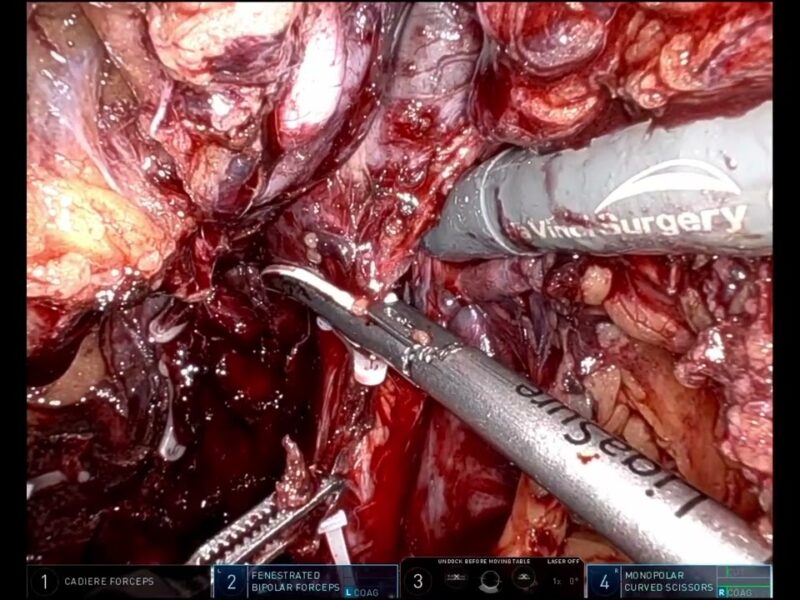
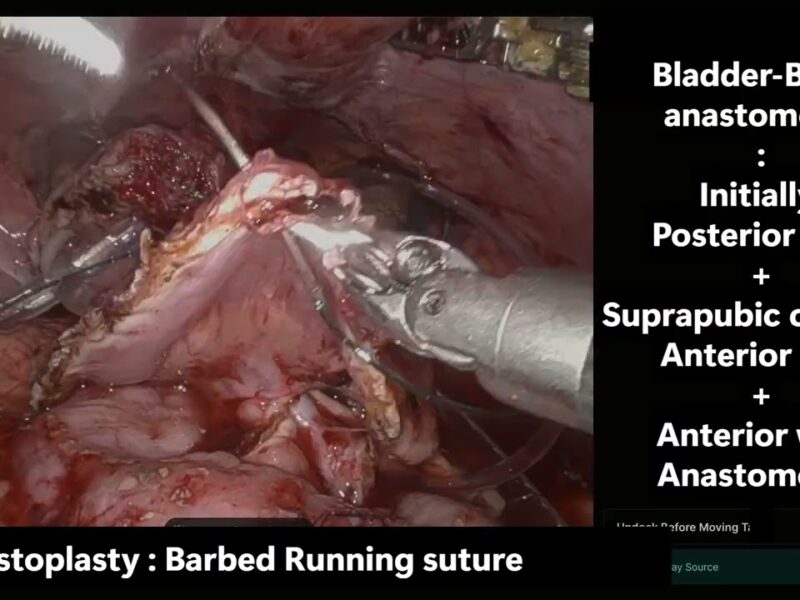
INTRODUCTION: A mobile, high-resolution PET/CT-imaging device (AURA 10 specimen PET/CT imager, XEOS Medical NV, Belgium), was used to guide robot-assisted radical prostatectomy (RARP) and pelvic lymph node dissection (PLND).
MATERIALS AND METHODS: to date, we performed three cases of RARP and PLND with intraoperative use of the specimen imager. Patients underwent preoperative staging with MRI and 68Ga-PSMA PET/CT for high-risk prostate cancer. During trocar placement, an intravenous injection of 68Ga-PSMA-11 (2 MBq/kg) was performed in the OR. Lymph nodes were immediately removed and scanned. After complete excision, the prostate was removed and PET/CT images were acquired to check for positive surgical margins (PSM). SUVmax of the scanned lymph nodes, background SUVMax and LN/background ratio (TBR) were calculated.
RESULTS: on average, the time required to scan each specimen was 12 minutes (SD 3). The median time between injection and specimen PET/CT imaging was 98 minutes for lymph nodes, and 3.8 hours for prostate. The average nodal yield was 17.3 (5.8 SD) nodes per patient, and only one node was positive. Specimen PET/CT images showed a focal uptake in a metastatic node (TBR 13.6), and no uptake or diffuse, faint uptake in negative nodes (TBR range: 1-5.3). Intraoperative PET/CT images allowed to detect negative surgical margins in two patients.
CONCLUSIONS: the intraoperative use of the specimen PET/CT imager is safe and feasible, and could improve the evaluation of prostate surgical margins and lymph node status, helping the surgeon to pursue the oncological radicality of the procedure while safely pushing the boundaries of a hyper-conservative surgery.
See more at: https://vattikutifoundation.com/videos/
Date
August 15, 2020