652 Intraoperative Visualization of Thoracic Duct, Primary Tumor, and Trachea
Dr. Jagdishwar Goud
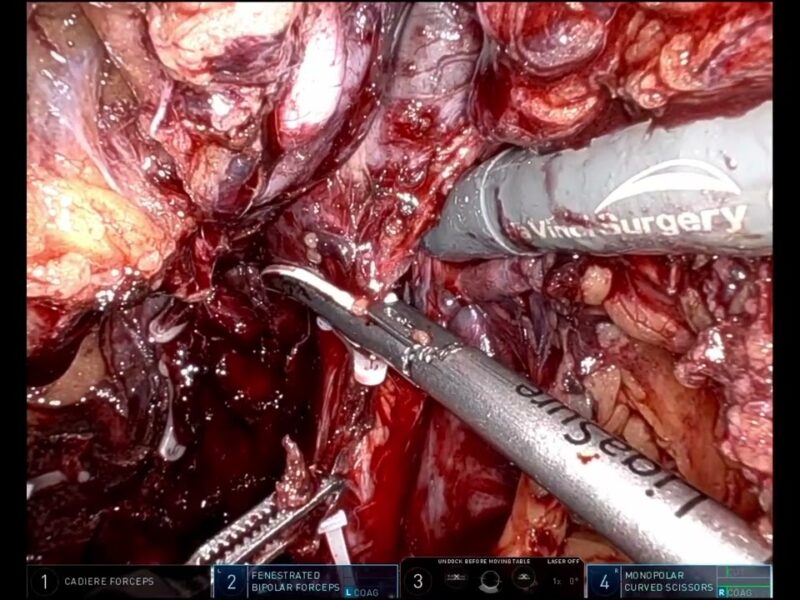
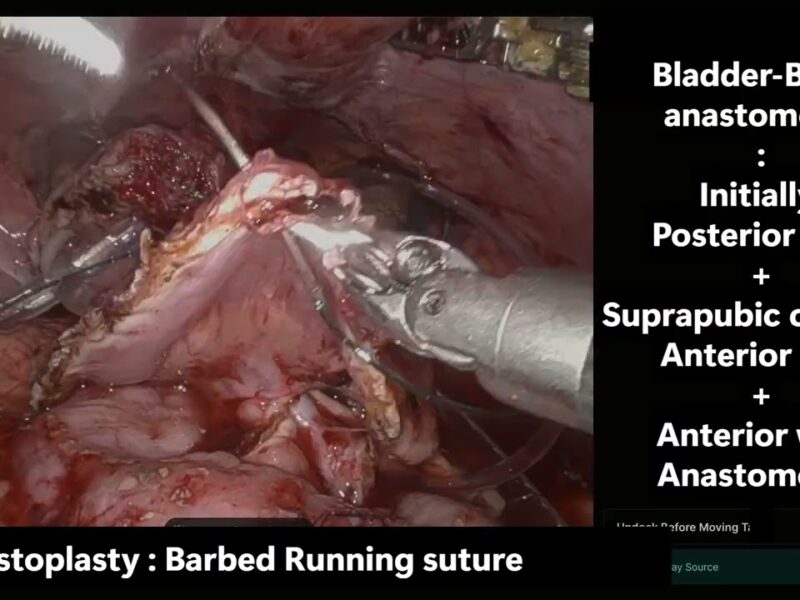
Esophagectomy is a most complex oncologic procedure, with high risks of thoracic duct injury leading to chyle leaks, tracheal injury, & incomplete tumor margin clearance. Identifying these vital structures is particularly difficult in patients with distorted anatomy after neoadjuvant therapy. Conventional robotic surgery provides magnified vision but still relies on subjective interpretation without real-time objective guidance. Solution: This study evaluated indocyanine green near-infrared fluorescence imaging integrated with the Firefly® robotic platform in 32 patients. A tailored multimodal approach was applied: ICG injection into inguinal lymph nodes for thoracic duct visualization, submucosal/EUS-guided injection for tumor localization, ICG nebulization for tracheobronchial mapping. This enabled reliable intraoperative identification of critical structures. Innovation: The study is the first to combine multiple ICG delivery routes within robotic esophagectomy, notably introducing airway nebulization for tracheal delineation. This novel fluorescence-guided navigation enhances surgical precision, safety, & opens pathways for selective nodal mapping in esophageal cancer.
Procedure Innovation, Cardiothoracic surgery, Esophagectomy, ICG
See more at: https://vattikutifoundation.com/videos/
Date
August 15, 2020