Robot-assisted radioguided surgery using a DROP-IN gamma probe
This video was entered By Drs. Paolo Dell’ Oglio & Matthias N. van Oosterom in the 2022 KS International Robotic Surgery Innovation Awards, sponsored by the Vattikuti Foundation. It was featured in the Vattikuti Symposium ‘Humans at the Cutting Edge of Robotic Surgery,’ held in Miami, Florida November 19, 2022.
Here is the Abstract:
Robot-assisted radioguided surgery using a DROP-IN gamma probe
Paolo Dell’Oglio *,1, Matthias N. van Oosterom *,2, Henk G. van der Poel3, Pim J. van Leeuwen3, Fijs W.B. van Leeuwen2
* Shared first presenters
1 Department of Urology, ASST Grande Ospedale Metropolitano Niguarda, Milan, Italy;
2 Interventional Molecular Imaging Laboratory, Department of Radiology, Leiden University Medical Center, Leiden, The Netherlands;
3 Department of Urology, Netherlands Cancer Institute-Antoni van Leeuwenhoek Hospital, Amsterdam, The Netherlands;
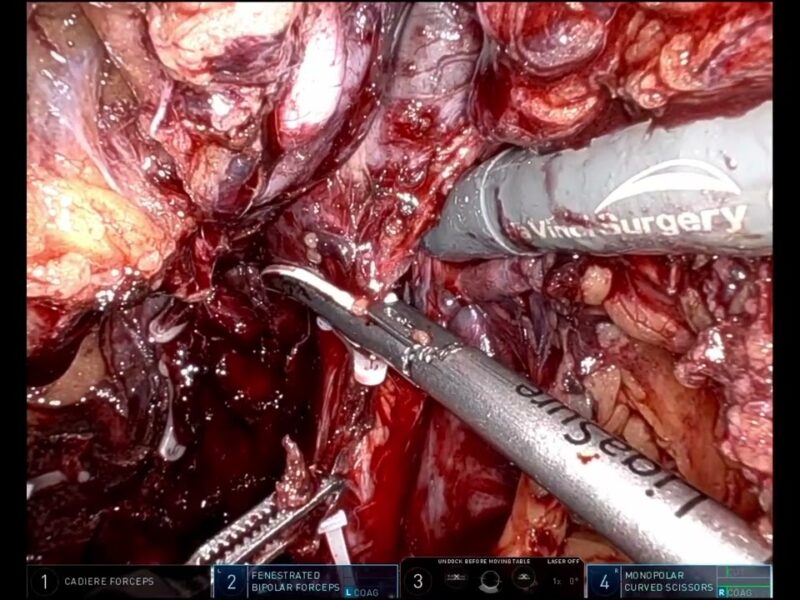
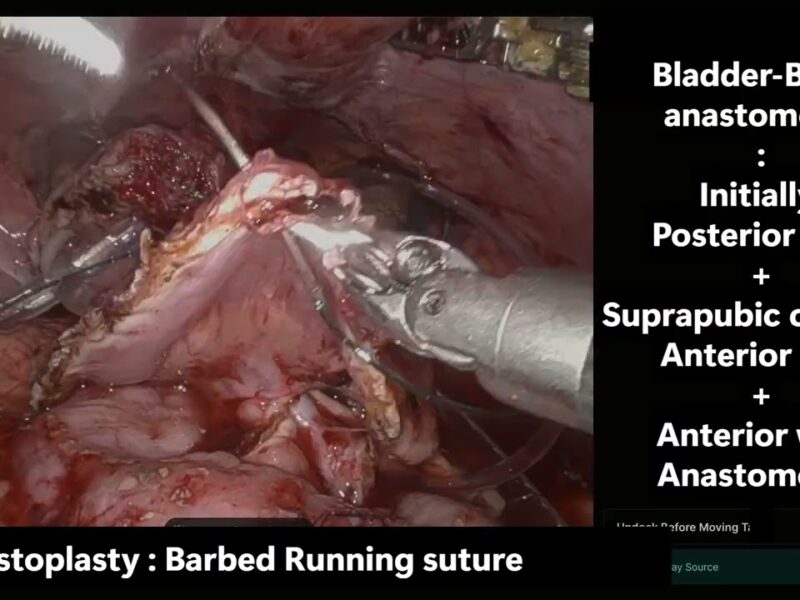
Aim: Robotic systems deliver many advantages for the minimal-invasive setting, especially for prostate cancer (PCa) management. However, they also give rise to specific challenges. For example, when applying radioguided surgery, the restricted access and the detachment of the robotic surgeon from the surgical field impairs the utility of traditional laparoscopic gamma-probes. To improve maneuverability and regain control for the surgeon, we designed and translated a tethered DROP-IN gamma-probe, evaluating it during both sentinel lymph node (SLN) and PSMA-targeted radioguided surgery.
Methods: We evaluated our image-guided surgery experience with the DROP-IN gamma- probe in greater than-65 patients with (recurrent) PCa. In the primary tumor setting, SLN resections were guided by ICG-99mTc-nanocolloid (both radioactive and fluorescent). PSMA-targeted salvage resections were guided by 99mTc-PSMA-I&S. Performance of intraoperative DROP-IN guidance was evaluated based on sensitivity, specificity and background activity of relevant tissues.
Results: In SLN procedures, the sensitivity and specificity of DROP-IN probe was 100%, superior to the traditional gamma-probe and fluorescence imaging. In PSMA-targeted surgery, sensitivity was 86% and specificity 100%. During the PSMA-targeted procedures, nodal count rates were about 5-times lower than for the SLN procedures. More interference was observed from background tissues (i.e., bladder, bowel, urine, blood). Ex-vivo evaluation of the specimens excised helped to confirm a successful lesion retrieval in all cases.
Conclusions: The DROP-IN technology has proven its potential for robotic radioguided SLN and PSMA-targeted surgery. Differences in tracer accumulation and tracer pharmacokinetics need to be accounted for, rendering in-vivo lesion localization different in a PSMA-targeted procedure relative to SLN procedure.
See more at: vattikutifoundation.com/videos
Date
August 15, 2020